The Nebraska Medical Center saw an opportunity during the programming phase of their future Comprehensive Cancer Center to rethink the surgery platform campus-wide. It was a major decision point in the programming project to analyze the current surgery suite locations, which could potentially encompass four separate spaces with the existing University Tower and Hixson-Lied Building and the addition of the new Comprehensive Cancer Center, Ambulatory Center and Eye Center. The goal of the project was to determine the optimal future location(s) for specific patient populations based on prioritized operational goals. Given the complexity and variation within the system, Discrete Event Simulation (DES) was deemed as the best tool for this analysis.

Campus-wide Surgery Planning Discrete Event Simulation
CUSTOMER
The Nebraska Medical Center
The Challenge
The Solution
Model Overview
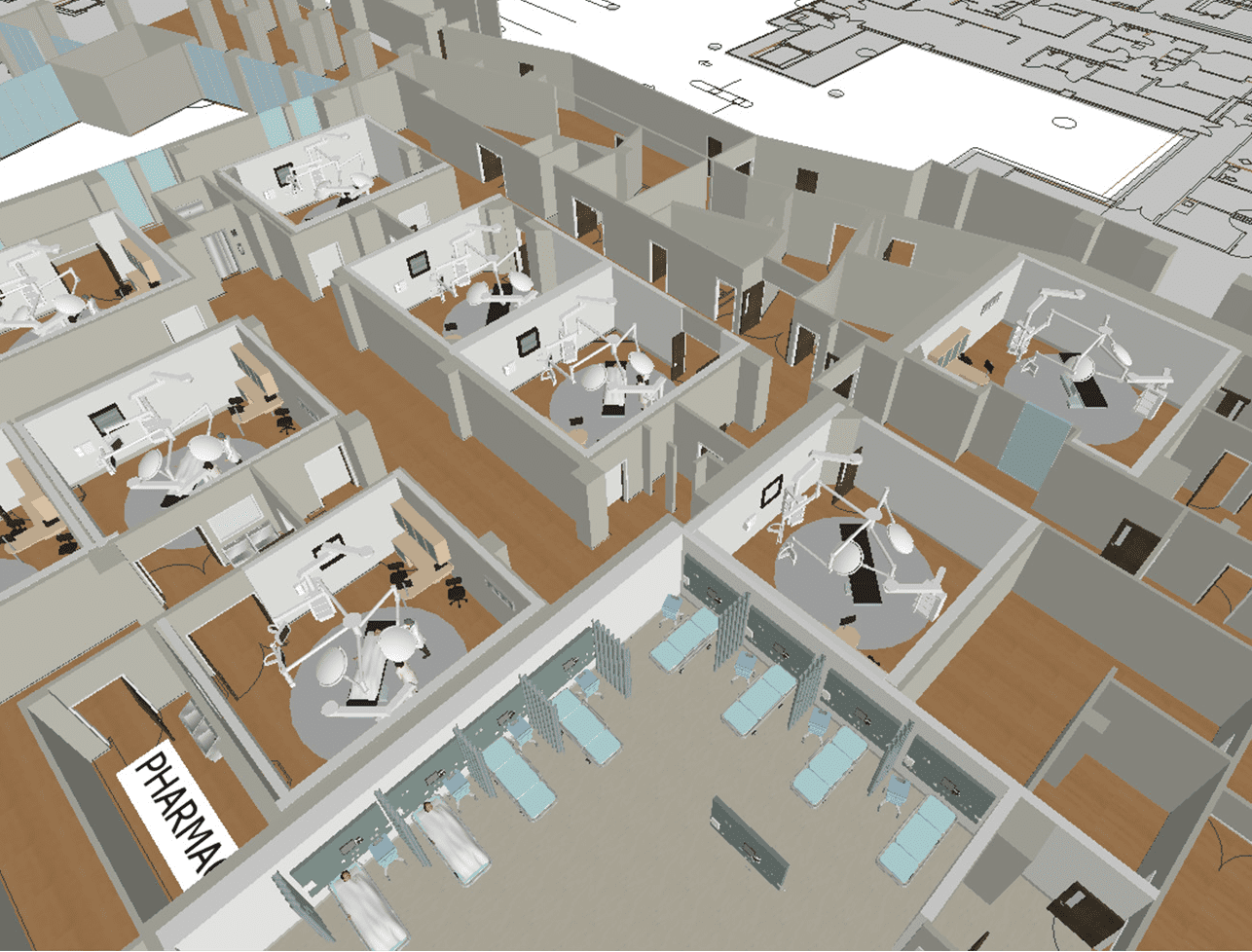
The simulation is a model (mathematical and logical) of the physical system that has changes at precise points in time. By partnering with TNMC user groups to map current processes as well as using TNMC’s current state information from both the Hospital Operating System as well as the Surgical Information System (actual arrival times, staffing models, resource utilization, durations, travel distances, etc.), our simulation software modeled the current state system and optimized it in a virtual environment to identify and reduce variation and bottlenecks prior to live implementation.
The creation of an expedited decision making reporting structure including:
- Operational Knowledge Team: day-to-day operational subject matter experts including staff, physicians, and information technology provided data and answers to workflow questions in near real-time.
- Accelerated Decision Team: operational leaders removed barriers in the process and made decisions regarding the simulation such as assumptions versus collection of real data.
- Surgical Services Steering Committee (SSSC): Perioperative Leadership made up of decision makers who had the authority to put decisions into practice immediately.
The team established a strict project scope, timeline, and prioritized metrics of success with the SSSC by which all decisions for this analysis would be made in conjunction with the overall project vision.
- Operating room utilization (75%-80%)
- Patient travel distance (minimize)
- Surgeon travel distance (minimize)
During current state DES modeling HDR worked with the Operational Knowledge Team to understand and map the current state workflow to a level of detail that allowed HDR to best model patient and staff behavior based on the following patient stratifications:
- Day Surgery, 23 Hour Surgery, Inpatient Surgery
- Surgical Service
- Cancer vs. Non-Cancer
A rigorous data collection plan was developed and the population of that plan along with manual data collection and appropriate assumptions began the development of the model. The model was then verified with NMC’s Subject Matter Expert (SME) Team and the SSSC for accuracy.
Future state DES modeling in combination with capacity modeling and growth projections modeled estimated hours for each surgical service by site for each of the scenarios in order to better inform the services future location based on a block schedule policy (for instance, will Vascular Surgery’s volumes warrant a block of time in the Ambulatory building within the next 10 years?). Ideal state operational assumptions were compared to TNMC’s current state metrics and verified with SSSC. Growth projections were completed for strategy neutral, strategy informed and strategy informed plus additional growth factor per approval by the SSSC.
HDR modeled the following Future State Scenarios based on this information both from a capacity modeling and DES perspective in order to compare and identify situations in which variation had the greatest impact on operations and facility planning. Each of these 7 scenarios was modeled 8 times considering both current and ideal operations as well as the four growth strategies. All models were validated and verified by the SME Team as well as the SSSC for accuracy of data and assumptions resulting in an unanimous selection that determined the future locations of all surgery suites, the number of ORs located in each suite, the services that would be performed at each location and the operations within each location. The selection was based on the Vision and Guiding Principles as well as the prioritized Metrics of Success.
The Business Impact
The Results
Six identified opportunities for improvement/outcomes were identified:
- Increased operating room utilization during staffed peak hours
- Decreased operating room utilization during non-peak hours
- Increased utilization of equipment specific rooms (resulting in a need for fewer total operating rooms)
- Reduced surgeon travel distances and frequency
- Reduced patient travel distances
- Reduced turnover times by services by patient type
By using both Capacity Modeling as well as DES in parallel as part of the programming process, the end result was a well tested projection that was based upon the actual operations (including variation) of TNMC as well as the forecasted volumes analysis. This allowed TNMC to directly connect strategy in programming through design to implementable operations, thus ensuring the most efficient future state model.
Applications