by Jason Ceresoli and Michael Kuhl (R.I.T.)
As presented at the 2018 Winter Simulation Conference
The treatment of patients in outpatient healthcare clinics is a continually growing trend as technology improves and recovery benefits are recognized. In this paper, we focus on the operational aspects of clinics that will impact clinic design decisions relative to productivity, efficiency, and quality of patient care. We develop a generalized Healthcare Clinic Design Simulator (HCD-Sim) to study the dynamic system behavior and to analyze alternative outpatient healthcare clinic designs. Our simulation framework is designed to have a data-driven structure that is able to represent a large class of outpatient healthcare clinics through the specification of clinic data relative to patient flows, work flows, and resource requirements. We describe our methodology and demonstrate the capabilities of experimentation utilizing the simulation framework.
Introduction
A main goal of healthcare organizations is to provide effective and efficient care. With this goal in mind, healthcare organizations have identified the necessity in analyzing and studying their systems and processes to improve operational performance. The design of healthcare facilities is one area that can impact the quality and effectiveness of care that patients receive. The number of treatment rooms, available equipment, and available physicians are a few of the many design choices that healthcare planners must determine when designing a system. Additionally, there have been several key healthcare trends that have increased the need for more carefully planned facilities; the focus on reduction of cost while increasing quality, the growing importance of improving patient satisfaction, and the shift in facility use to more outpatient care (Ulrich 2001). Poorly designed healthcare facilities cultivate environments that can cause long patient waits and congestions which can result in increased stress for healthcare staff (Rohleder et al. 2011), and ailments that were commonly treated via inpatient settings are transitioning to outpatient settings due to significant reduction in costs, increased patient quality of life, and decreased chance for hospital acquired infections (Vaughn et al. 2016). Addressing issues that arise from poorly designed facilities can have a great impact on the operational performance (Ulrich et al. 2008). For these reasons, healthcare centers are now being designed to consider the new demands for outpatient treatments.
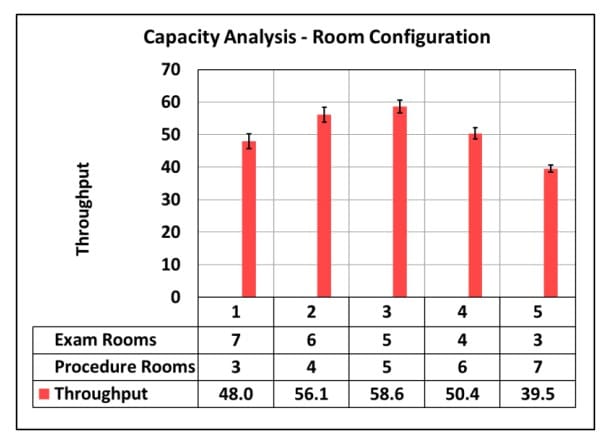
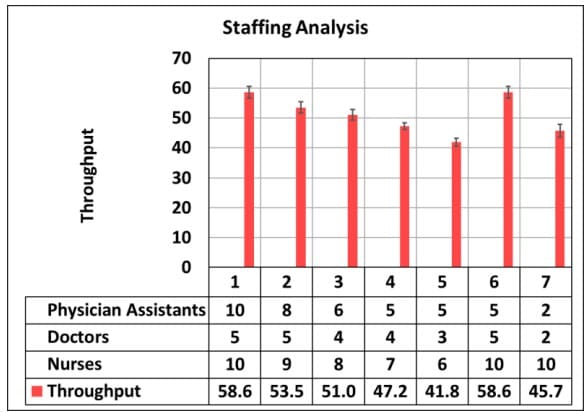
The objective of this research is to develop a simulation framework for healthcare clinics to analyze their system from an operational perspective. The framework will be general enough so that its use can be applied to different clinics but detailed enough to accurately model the dynamic and complex nature of the clinical operations. The framework can be used as a tool to help healthcare planners make more informed choices by understanding the impact a decision has on performance measures of interest. The framework will support capacity and patient flow analyses to provide decision makers a method to identify limitations on a healthcare system, and to also identify the key parameters that have the most impact on performance.
This enhanced understanding will enable the best design to be identified in a low cost and low risk environment. The remainder of this paper is organized as follows: a summary of related work is presented in Section 2; the simulation framework methodology is discussed in Section 3; experimentation using the framework is shown in Section 4; and a conclusion and future work are discussed in Section 5.
Summary of related work
The use of simulation to study healthcare systems has grown substantially in the last several years. In this section, we summarize a portion of this research related to the need for generalized/reusable models; the use of simulation to investigate capacity analysis and patient flow in healthcare; and finally, the application of simulation to study outpatient clinics.
Researchers have shown that discrete-event simulation is capable of modeling complex systems, making it advantageous to use when analyzing healthcare systems (Hong et al. 2013; Roberts 2011). Further, reusable models in healthcare are needed as advancements of simulation in healthcare is stunted due to the tendency to start models from scratch, rather than implement general simulation concepts (Günal and Pidd 2010; Mahdavi et al. 2013; Robinson et al. 2004; Roberts 2011).
Capacity analysis and patient flow are two areas central to simulation research in healthcare. Simulation is used extensively for capacity analysis because of the opportunity simulation provides to replicate and evaluate a system in a low cost and low risk environment (Katsaliaki and Mustafee 2011). In a comprehensive review of capacity and performance of healthcare services, Jack and Powers (2009) found that unlike other service industries, the consequences for failing to appropriately match the patients demand to the scarce resources is severe. Furthermore, capacity decisions are associated with the allocation ofscarce resources to handle demand which can impact the quantity of care that can be delivered and the mix of patients the system is capable of treating (Smith-Daniels et al. 1988). Application of capacity analysis have included studies of emergency departments (Oh et al. 2016); a cancer treatment center (Romero et al. 2013); hospitals bed requirement (Harper and Shahani 2002): and an outpatient orthopedic clinic (Baril et al. 2014). In addition to capacity analysis, patient flow and care pathways are the center of many studies, as they can lead to opportunities for performance improvement (Marshall et al. 2005). Cote (2000) argues that patient flow and capacity are tightly coupled as patient flow is effectively the demand imposed on a healthcare system. In addition, McLaughlin and Hays (2008) indicate that analyzing patient flow allows the identification of non-value added activities which if removed can lead to efficiency gains
From an operational perspective, a continuing trend in healthcare delivery is the shift to treating patients in outpatient settings, rather than solely inpatient (Cote 2000). Over the past two decades, healthcare systems have noticed an almost doubling of the number of outpatient visits (Parks et al. 2011). The motivation for this recent trend is believed to be from innovation in medication, technological advances, procedures (Cote 2000) and a reduction in financial cost (Vaughn et al. 2016). However, many of the problems that have plagued inpatient departments (congestion, staff overtime, high waiting times, etc.) have carried over to outpatient clinics. Hong et al. (2013) explains these issues in outpatient clinics lead to increase in patient dissatisfaction. The is important as patient satisfaction impacts the reimbursements a healthcare system receives from Medicare and Medicaid (Kennedy et al. 2014).
Building on this research, we aim to help address the issues of designing and analyzing effective and efficient outpatient clinics by developing a generalized simulation modeling framework. The reusable modeling approach will allow for capacity and patient flow analysis for the purpose of decision-making. The novelty of our modeling framework is how it expands upon the DEVs formulism and allows for scalability of atomic models (Zeigler et al. 2000). Additionally, this framework builds off the work proposed by Pérez et al. (2010), Alvarado et al. (2018), and Abo-Hamad and Arisha (2013) by enabling the components or atomic models that represent the clinic attributes (treatment rooms, staff, patient flows, etc.) to be altered by inputs driven through a data table. Moreover, the number of these attributes can be changed by data table inputs thus reducing the time required to model different clinics or alternative designs.