by Mandvi Malik and Dusan Sormaz (Ohio University)
As presented at the 2017 Winter Simulation Conference
In the past few decades, simulation in healthcare has gained immense attention from researchers because of its ability to detect problems that help in the improvement of the facility. It is important for any healthcare to know how many beds, nurses, and therapist they need in their facility to improve their service. In this research, we have created a customized object that is used to design simulation model for progressive care unit in a hospital. The objective of this research is to a make a flexible simulation model that can easily be extended and re used to make simulation model for any facility. The simulation model built would help the health care personnel in determining the number of beds, therapists and nurses in their facility.
1 Introduction
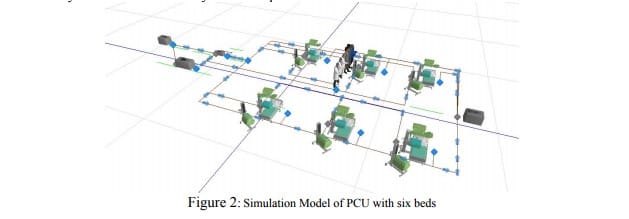
“A simulation model is a representation that incorporates time and the changes that occur over time” [1]. Simulation can help the health care companies in utilizing their resources suitably. Using simulation they can decide if they need to increase a number of beds or need to increase a number of therapists in their facility. In the past, researchers have used simulation as a decision making tool for improving the health care facilities [2] However, simulation models built in the past were mostly flat simulation models and were built using the objects from the standard library supplied by software. In this research, we have created a new customized object which handles all the patient procedures during his/her stay at Progressive Care Unit (PCU). The customized object is re-usable. The customized object is extended and combined to create a complete simulation model of the PCU unit. The model is built using Simio [3].
2 Progressive care unit (PCU)
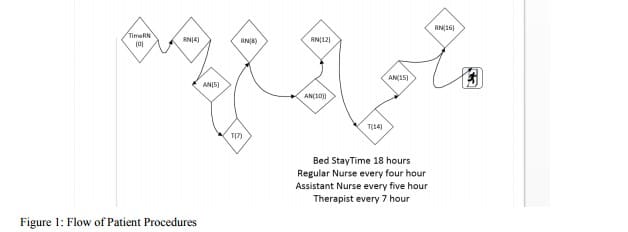
The patients come to PCU for post-procedural care from various other departments in the medical center. The departments may be an emergency department, ICU, surgery, or direct admissions. The duration of patients stay in the PCU depends on their acuity levels: low, medium and high acuity levels. The patients are accompanied by a regular nurse to their beds when they arrive. During a patient stay, he/she is assigned to a regular nurse, a therapist and an assistant nurse. They perform three different procedures: treatment by the therapist, regular nurse rounding, and assistant nurse rounding multiple times during a patient stay in the unit (with regular intervals).The patient leaves the PCU when his/her stay time expires in the PCU, meaning that they recovered.