by Jason Ceresoli and Michael Kuhl (R.I.T.)
As presented at the 2018 Winter Simulation Conference
Abstract
The treatment of patients in outpatient healthcare clinics is a continually growing trend as technology improves and recovery benefits are recognized. In this paper, we focus on the operational aspects of clinics that will impact clinic design decisions relative to productivity, efficiency, and quality of patient care. We develop a generalized Healthcare Clinic Design Simulator (HCD-Sim) to study the dynamic system behavior and to analyze alternative outpatient healthcare clinic designs. Our simulation framework is designed to have a data-driven structure that is able to represent a large class of outpatient healthcare clinics through the specification of clinic data relative to patient flows, work flows, and resource requirements. We describe our methodology and demonstrate the capabilities of experimentation utilizing the simulation framework.
Introduction
A main goal of healthcare organizations is to provide effective and efficient care. With this goal in mind, healthcare organizations have identified the necessity in analyzing and studying their systems and processes to improve operational performance. The design of healthcare facilities is one area that can impact the quality and effectiveness of care that patients receive. The number of treatment rooms, available equipment, and available physicians are a few of the many design choices that healthcare planners must determine when designing a system. Additionally, there have been several key healthcare trends that have increased the need for more carefully planned facilities; the focus on reduction of cost while increasing quality, the growing importance of improving patient satisfaction, and the shift in facility use to more outpatient care (Ulrich 2001). Poorly designed healthcare facilities cultivate environments that can cause long patient waits and congestions which can result in increased stress for healthcare staff (Rohleder et al. 2011), and ailments that were commonly treated via inpatient settings are transitioning to outpatient settings due to significant reduction in costs, increased patient quality of life, and decreased chance for hospital acquired infections (Vaughn et al. 2016). Addressing issues that arise from poorly designed facilities can have a great impact on the operational performance (Ulrich et al. 2008). For these reasons, healthcare centers are now being designed to consider the new demands for outpatient treatments.
The objective of this research is to develop a simulation framework for healthcare clinics to analyze their system from an operational perspective. The framework will be general enough so that its use can be applied to different clinics but detailed enough to accurately model the dynamic and complex nature of the clinical operations. The framework can be used as a tool to help healthcare planners make more informed choices by understanding the impact a decision has on performance measures of interest. The framework will support capacity and patient flow analyses to provide decision makers a method to identify limitations on a healthcare system, and to also identify the key parameters that have the most impact on performance.
This enhanced understanding will enable the best design to be identified in a low cost and low risk environment. The remainder of this paper is organized as follows: a summary of related work is presented in Section 2; the simulation framework methodology is discussed in Section 3; experimentation using the framework is shown in Section 4; and a conclusion and future work are discussed in Section 5.
Summary of related work
The use of simulation to study healthcare systems has grown substantially in the last several years. In this section, we summarize a portion of this research related to the need for generalized/reusable models; the use of simulation to investigate capacity analysis and patient flow in healthcare; and finally, the application of simulation to study outpatient clinics.
Researchers have shown that discrete-event simulation is capable of modeling complex systems, making it advantageous to use when analyzing healthcare systems (Hong et al. 2013; Roberts 2011). Further, reusable models in healthcare are needed as advancements of simulation in healthcare is stunted due to the tendency to start models from scratch, rather than implement general simulation concepts (Günal and Pidd 2010; Mahdavi et al. 2013; Robinson et al. 2004; Roberts 2011).
Capacity analysis and patient flow are two areas central to simulation research in healthcare. Simulation is used extensively for capacity analysis because of the opportunity simulation provides to replicate and evaluate a system in a low cost and low risk environment (Katsaliaki and Mustafee 2011). In a comprehensive review of capacity and performance of healthcare services, Jack and Powers (2009) found that unlike other service industries, the consequences for failing to appropriately match the patients demand to the scarce resources is severe. Furthermore, capacity decisions are associated with the allocation ofscarce resources to handle demand which can impact the quantity of care that can be delivered and the mix of patients the system is capable of treating (Smith-Daniels et al. 1988). Application of capacity analysis have included studies of emergency departments (Oh et al. 2016); a cancer treatment center (Romero et al. 2013); hospitals bed requirement (Harper and Shahani 2002): and an outpatient orthopedic clinic (Baril et al. 2014). In addition to capacity analysis, patient flow and care pathways are the center of many studies, as they can lead to opportunities for performance improvement (Marshall et al. 2005). Cote (2000) argues that patient flow and capacity are tightly coupled as patient flow is effectively the demand imposed on a healthcare system. In addition, McLaughlin and Hays (2008) indicate that analyzing patient flow allows the identification of non-value added activities which if removed can lead to efficiency gains
From an operational perspective, a continuing trend in healthcare delivery is the shift to treating patients in outpatient settings, rather than solely inpatient (Cote 2000). Over the past two decades, healthcare systems have noticed an almost doubling of the number of outpatient visits (Parks et al. 2011). The motivation for this recent trend is believed to be from innovation in medication, technological advances, procedures (Cote 2000) and a reduction in financial cost (Vaughn et al. 2016). However, many of the problems that have plagued inpatient departments (congestion, staff overtime, high waiting times, etc.) have carried over to outpatient clinics. Hong et al. (2013) explains these issues in outpatient clinics lead to increase in patient dissatisfaction. The is important as patient satisfaction impacts the reimbursements a healthcare system receives from Medicare and Medicaid (Kennedy et al. 2014).
Building on this research, we aim to help address the issues of designing and analyzing effective and efficient outpatient clinics by developing a generalized simulation modeling framework. The reusable modeling approach will allow for capacity and patient flow analysis for the purpose of decision-making. The novelty of our modeling framework is how it expands upon the DEVs formulism and allows for scalability of atomic models (Zeigler et al. 2000). Additionally, this framework builds off the work proposed by Pérez et al. (2010), Alvarado et al. (2018), and Abo-Hamad and Arisha (2013) by enabling the components or atomic models that represent the clinic attributes (treatment rooms, staff, patient flows, etc.) to be altered by inputs driven through a data table. Moreover, the number of these attributes can be changed by data table inputs thus reducing the time required to model different clinics or alternative designs.
Simulation of healthcare clinics
In this section, we summarize the operational aspects of outpatient healthcare clinics, and the translation of these aspects to the development of a generalized simulation framework. In particular, our focus is on the operational aspects of the clinic that will impact clinic design decisions relative to productivity, efficiency, and quality of patient care. These include aspects such as facility layout and configuration, patient arrival patterns, patient flows, and work flows, among others. To represent the dynamic behavior and performance, a discrete-event simulation framework is presented to facilitate system design, analysis, and decisionmaking.
Clinic System Description
While there are a plethora of specialty outpatient healthcare clinics, from an operational perspective, most share a similar operational flow and sequence. Although the specific details with regard to medical diagnosis and treatment may differ, we describe a representative clinic from patient flow, and work flow perspectives.
Patients arrive to a clinic either based on a schedule, as walk-ins, or a combination of both. Patients can typically be classified by their diagnosis or reason for the visit and thus defining their patient care pathway. At arrival, the patient checks in (often at a reception desk) and the clinic staff is notified that the patient is waiting. From the staff perspective, the patient arrival triggers the staff to determine who will be assigned to that patient. Once a staff member has selected the patient, they will begin reviewing the patient’s records. Meanwhile, the clinic determines the availability of an exam room for the patient. Once available, the patient will have their vital signs taken on the way to the exam room. In the exam room, various assessments or procedures will occur. Typically these include a preliminary assessment from a nurse of physician’s assistant followed by a doctor assessment or procedure. Between those assessments a handoff occurs to brief the doctor on the findings from the preliminary assessment. If the patient required a procedure, depending on the procedure and the resource requirements, the procedure could either be performed in the exam room or in a separate procedure room (this may depend on the procedure required and/or room availability.). Once the patient has finished with their care, they will check out and depart the system. After the patient departs, the staff finish the charting and order writing, if required, before seeing the next patient. (A flowchart illustrating patient flows is shown in Figure 2 for the representative healthcare clinic used in our experiment.)
Healthcare Clinic Simulation Framework
To provide a generalized method to study the dynamic behavior of healthcare clinics and to analyze alternative outpatient healthcare clinic designs, we have developed a Healthcare Clinic Design Simulator (HCD-Sim). Our simulation framework is designed to have a data-driven, modular structure. That is, our intent is to provide a discrete-event simulation model that will be able to represent a large class of outpatient healthcare clinics only through the specification of clinic data relative to patient flows, work flows, and resource requirements. While ongoing research is continuing the framework can conceptually be divided into the following five components – (a) clinic system inputs; (b) clinic decision variables; (c) flexible clinic model; (d) experimental design; and (e) clinical performance. The overall simulation framework for HCDSim is presented in Figure 1.
HCD-Sim utilizes the operational data that defines the clinic as user-specified inputs. The clinical system input includes the patient types, patient mix, arrival schedule, and patient flow pathways. Patient types from the perspective of the simulator refers to different flows that a patient could take through the clinic. This will include the resources that are required for their care along with the processing times for assessments, treatments, and associated processes.
The clinic decision variables define the set of design decisions that the healthcare clinic is interested in investigating such as staffing, equipment, clinical design specifications, and prioritizations. The staffing variables may include the staffing levels and schedules for staff. The equipment variables may include the number of medical devices or capacity of the equipment. The clinical design parameters refer to the number of exam and procedure rooms along with the sizing of wait and/or work rooms, etc. In addition, how the clinic prioritizes patients and how staff prioritize tasks are included as potential decision variables.
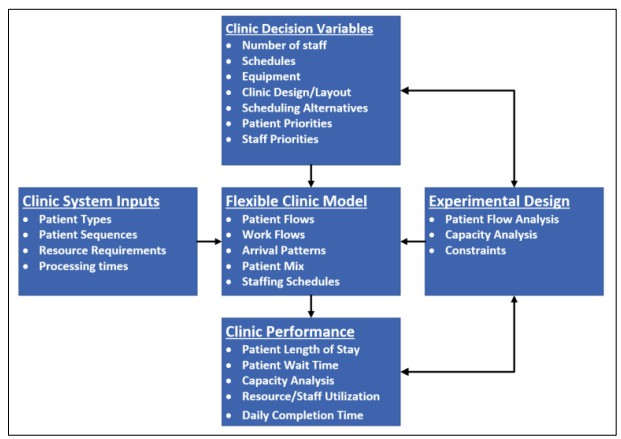
Figure 1: HCD-Sim modeling framework for the design and analysis of healthcare clinics.
The flexible clinic model takes the inputs and decision variables and creates a representative model of the clinic so that the decision variables can be studied through experimentation. The flexible clinic model is designed around a relational table architecture. The architecture enables the complex nature of patient flows and the resources to be modeled in a manner that is flexible and able to represent a large class of outpatient healthcare clinics. For example, multidisciplinary care teams can be included to model patient centered operations through the use of different types of staff treating the patient. The clinic model also includes a flexible structure for modeling the work flows, patient arrival patterns, patient mix, staffing schedules, and other system components.
The experimental design component, as shown in Figure 1, is linked to the decision variables that are being studied as well as the performance metrics. The experiments that the framework is currently designed to perform include patient flow analysis, capacity analysis, and resource optimizations. Patient flow can be analyzed to reduce non-value added steps and analyze the time a patient has to remain in the clinic to receive treatment. Capacity analysis of the clinic can be used to identify the limiting factors of system performance and productivity. And, resource optimization can be performed to determine the best mix of system resources (rooms, equipment, personnel, etc.) in order to optimize system performance.
Finally, clinic performance can be assessed by the simulation framework utilizing performance metrics related to productivity, efficiency, and quality of patient care. The performance metrics that the framework currently collects includes patient waiting times, resource utilization, staff utilization, staff overtime, congestion measures (queuing metrics), total time patient is in the system, and throughput, among others. HCD-Sim is currently implemented using Simio simulation software. The design of the framework heavily utilizes the relational database table structure to enable the data-driven clinic specification of the clinic parameters, operational flows, and decision variables.
Experimention using hcd-sim
To demonstrate the capabilities of experimentation with the HCD-Sim framework, an experiment on the design and capacity analysis of a representative, general outpatient clinic is considered. In particular, this experiment will explore questions related to facility configuration, staffing levels, and patient mix with regard to the clinical capacity measured in terms of patient throughput. These questions include:
- What is the impact of the mix of the number of exam rooms and procedure rooms on clinic
- For a given facility configuration, how does the number of medical personnel (nurses, doctors, and physician assistants) effect clinic capacity?
- What effect does the mix of patients types (based on patient flow pathway) have on clinic capacity?
Although HCD-Sim can produce a comprehensive array of system performance measures and statistics, we have elected to focus on patient throughput to illustrate the types of analysis one can perform using the simulation framework.
Clinic Operations
The clinic facility and operations of the representative outpatient clinic used in the experiment include the following. The layout of the clinic consists of a check-in/check-out station, waiting room, vital signs assessment station, exam rooms, procedure rooms, and staff work room/stations. There are six different patient types that visit this clinic. The six patient types differ in the resources that they require for their treatment and the procedures that are performed. The patient types along with their sequences and staff requirements are shown in Table 1.
Table 1: Patient flow sequences, resources requirements and process time durations for the general clinic. All duration times provided in minutes.
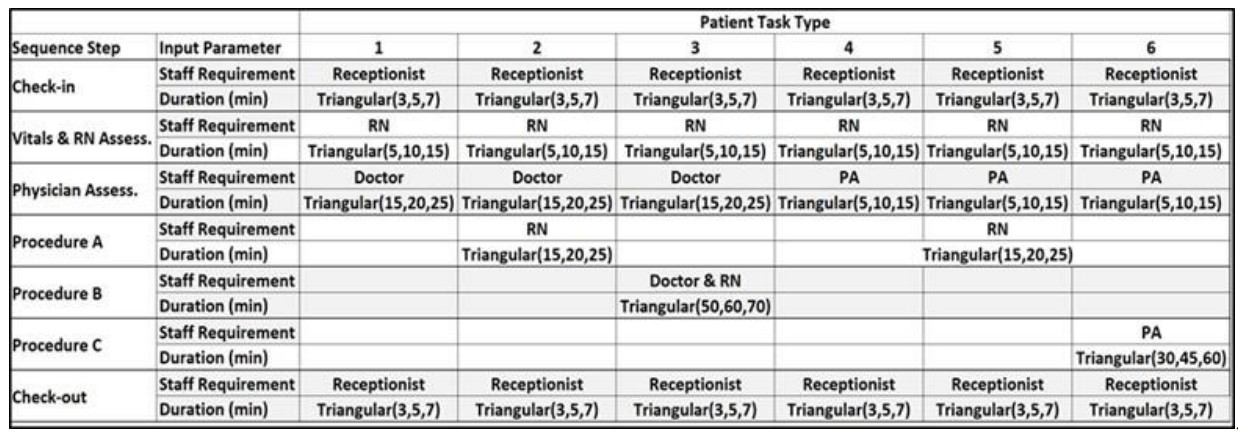
Patients flow through the clinic as shown in Figure 2. When a patient arrives, they check in and stay in a waiting room until an exam room is available. Once available, a nurse escorts the patient to the exam room and performs a general assessment. The nurse will leave the exam room and review the patient with the doctor or physician assistant (PA) in the staff work room. The physician then meets the patient and provides an assessment. After all the assessments are complete, the patient either checks out and leaves the clinic, or has a procedure completed with a physician, and/or nurse. When the procedure is complete, the patient leaves the clinic.
To test the theoretical limits of the clinic capacity, the patients arrive individually according to an event
that is triggered once the previous patient has finished the check in step. While not completely
representative of clinic operations, this method allows for an infinite stream of patients so the demand and
capacity limits can be assessed when altering the staff and room resources of the clinic.

Figure 2: Patient flow logic for the general clinic.
Experimental Setup
The decision variables under consideration for this experiment are the number of exam rooms and procedure rooms, staffing levels, and patient mix. The experiment will be conducted in three stages utilizing throughput as the primary performance measure of interest. First, the clinic is examined to determine the best combination of exam and procedure rooms subject to a space limitation of 10 total rooms and no constraints on staff where all patient types are equally likely. Next, the staffing levels are investigated using the best room combination from the first experiment. Finally, the patient mix is studied by varying the patient mix under the best room and staffing combination. The experimental results for these three stages are presented and discussed in the next section.
Experimental Results
The experimental results for the three staged experiments were collected using 25 independent replication of 10 hour clinic days. This three staged experimental method was used to systematically identify the impact of each decision variable (number or rooms, staffing levels, and patient mix). The capacity analysis for room configuration was performed for five different room configurations. The results are shown in Figure 3. These results show the configuration highest patient throughput results where there is an even split of 5 exam and 5 procedure rooms. Furthermore, this analysis provides data to suggest that exam rooms are more impactful on throughput than procedure rooms. In the subsequent experiments, the patient mix will be examined.
Given the 5 exam room/5 procedure room configuration, we assess the impact of different staffing levels on the performance of the clinic. In particular, seven staffing combinations are selected and compared based on average clinic throughput. The results for this staffing analysis are shown in Figure 4. Of the staffing configurations examined, the configuration of 5 physician assistants, 5 doctors, and 10 nurses was able to achieve the same average throughput of 58.6 patients per day as the non-personnel constrained experiment.
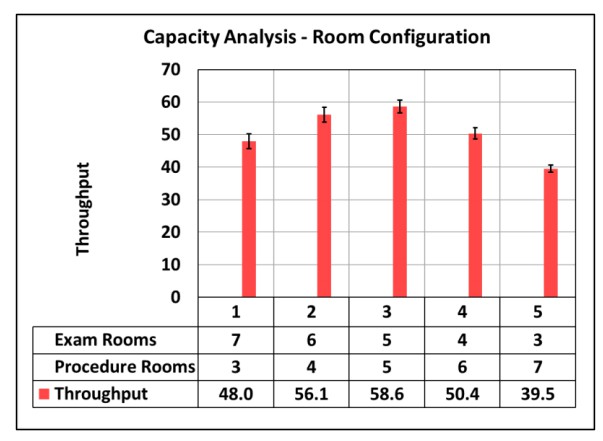
Figure 3: Capacity analysis results for possible room configurations.
The final experiment investigates the impact of different patient mix on capacity performance of the clinic. The experiment is conducted using the best combination of rooms (Combination 3 in Figure 3) and combination 6 in the staffing analysis. To assess the impact of different scheduling policies, five patient mix combinations are tested. The five combinations are selected to investigate the impact of the three procedures that are performed at the clinic. The results are shown in Figure 5. Combination 1 is the base case which is identical to results from the previous experiments. Combination 2 s increases the percentage of patients that require procedures, which corresponds to the lower throughput as compared to the base case. Combination 3 increases the two patient task types that have significantly longer procedures (B and C). Combination 4 is the inverse of combination 3, which intuitively, has the highest throughput since the longer procedures are less likely to be required. Finally, combination 5 investigates the throughput when patients arriving to the clinic require the doctor more than the physician assistant. Looking at all 5 combinations, the results are reasonable. This information could be useful for the clinic in the future to prevent scheduling patients in a manner that would restrict the flow of patients and reduce throughput.
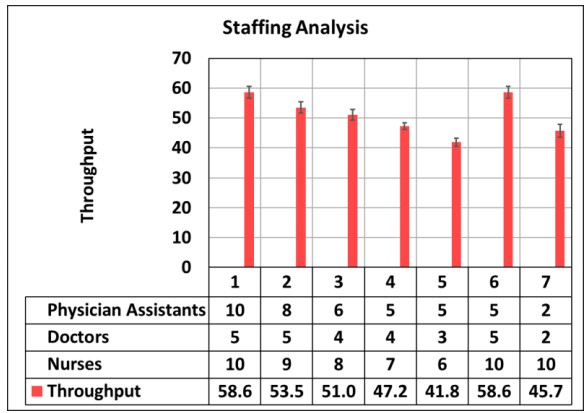
Figure 4: Staffing analysis results for different staffing configurations.

Figure 5: Patient mix analysis for seven different patient mix configurations.
Conclusion
In this paper a generalized simulation framework for the analysis of outpatient healthcare clinics, HCDSim, is introduced. The simulation framework is designed to provide a flexible platform for modeling and simulating a large class of outpatient healthcare clinics using a data-driven modeling technique. A representative clinic example demonstrates the framework and illustrates the analysis capability of the framework. HCD-Sim presents a step forward in data-driven and generalized healthcare simulation modeling techniques that could enable simulation to be used more widely among healthcare organizations without the time and effort required to construct a simulation model from scratch but yet effective enough to provide meaningful results for the purpose of decision-making.
Future work for this research and simulation framework includes the addition of financials to incorporate the budgetary constraints that face healthcare systems. Including these aspects will allow healthcare organizations to better evaluate the cost-benefit trade-offs among alternatives. Additionally, the framework could be expanded by enabling the components or attributes of the clinic to be dynamically created to further reduce the modeling required for alternative clinic designs.
Author biographies
JASON D. CERESOLI is a Masters student of the Department of Industrial and Systems Engineering at the Rochester Institute of Technology, Rochester, NY. He holds a bachelors degree in Industrial and Systems Engineering from the Rochester Institute of Technology. His research interest include discreteevent simulation and healthcare. His email address is jdc1625@rit.edu.
MICHAE E. KUHL is a professor in the Department of Industrial and Systems Engineering at Rochester Institute of Technology. He earned his Ph.D. in Industrial Engineering from North Carolina State University. His research interests include modeling and simulation of stochastic arrival processes, and the application of simulation and simulation-based optimization to systems including healthcare, manufacturing, cyber security, and project management. He is a member of the WSC Board of Director representing the INFORMS Simulation Society. He has also served WSC as Proceedings Editor (2005), Program Chair (2013), and Mobile App Chair (2014-2018). His e-mail address is Michael.Kuhl@rit.edu.
References
Abo-Hamad, W., A. Arisha. 2013. “Simulation-based Framework to Improve Patient Experience in an Emergency Department”. European Journal of Operations Research 224(1):154-166
Alvarado, M. M., T. G. Cotton, L. Ntaimo, E. Pérez, and R. Carpentier. 2018. “Modeling and Simulation of Oncology Clinic Operations in Discrete Event System Specification”. Simulation 94(2):105-121.
Baril, C., V. Gascon, and S. Cartier. 2014. “Design and Analysis of an Outpatient Orthopedic Clinic Performance with Discrete Event Simulation and Design of Experiments”. Computers & Industrial Engineering 78(2):285-298
Cote, M. J. 2000. “Understanding Patient Flow”. Decision Line 31(2):8-10.
Günal, M. M. and Pidd, M. 2010. “Discrete Event Simulation for Performance Modelling in Healthcare: A Review of the Literature”. Journal of Simulation 4(1):42-51.
Harper, P. R. and A. Shahani. 2002. “Modelling for the Planning and Management of Bed Capacities in Hospitals”. Journal of the Operational Research Society 53(1):11-18.
Hong, T. S., P. P. Shang, M. Arumugam, and R. M. Yusuff. 2013. “Use of Simulation to Solve Outpatient Clinic Problems: A Review of the Literature”. South African Journal of Industrial Engineering 24(3):27-47.
Jack, E. P. and T. L. Powers. 2009. “A Review and Synthesis of Demand Management, Capacity Management and Performance in Health-care Services”. International Journal of Management Reviews 11(2):149-174.
Katsaliaki, K. and N. Mustafee. 2011. “Applications of Simulation within the Healthcare Context”. Journal of the Operational Research Society 62(8):1431-1451.
Kennedy, G. D., S. E. Tevis, and K. C. Kent. 2014. “Is there a Relationship between Patient Satisfaction and Favorable Outcomes?”. Annals of Surgery 260(4):591-592.
Mahdavi, M., T. Malmström, J. van de Klundert, S. Elkhuizen, and J. Vissers. 2013. “Generic Operational Models in Health Service Operations Management: A Systematic Review”. Socio-Economic Planning Science 47(4):271-280.
Marshall, A., C. Vasilakis, C. and E. El-Darzi. 2005. “Length of Stay-based Patient Flow Models: Recent Developments and Future Directions”. Health Care Management Science 8(3):213-220.
McLaughlin, D. B. and J. M. Hays. 2008. Healthcare Operations Management. Washington, D.C: Health Administration Press
Oh, C., A. M. Novotny, P. L. Carter, R. K. Ready, D. D. Campbell, and M. C. Leckie. 2016. “Use of a Simulation-based Decision Support Tool to Improve Emergency Department Throughput”. Operations Research for Health Care 9:29-39.
Parks, J. K., P. Engblom, E. Hamrock, S. Satjapot, and S. Levin. 2011. “Designed to Fail: How Computer Simulation can Detect Fundamental Flaws in Clinic Flow”. Journal of Healthcare Management 56(2):135-146.
Pérez, E., L. Ntaimo, C. Bailey, and P. McCormack. 2010. “Modeling and Simulation of Nuclear Medicine Patient Service Management in DEVS”. Simulation 86(8-9):481-501.
Roberts, S. D. 2011. “Tutorial on the Simulation of Healthcare Systems”. In Proceedings of the 2011 Winter Simulation Conference, edited by S. Jain et al., 1408–1419. Piscataway, New Jersey: IEEE.
Robinson, S., R. E. Nance, R, J. Paul, M. Pidd, and S. J. E. Taylor. 2004. “Simulation Model Reuse: Definitions, Benefits and Obstacles”. Simulation Modelling Practice and Theory 12(7):479-494.
Rohleder, T. R., P. Lewkonia, D. P. Bischak, P. Duffy, and R. Hendijani. 2011. Using Simulation Modeling to Improve Patient Flow at an Outpatient Orthopedic Clinic”. Health Care Management Science 14(2):135-145.
Smith-Daniels, D. E., V. L. Smith-Daniels, and S. B. Schweikhart. 1988. “Capacity Management in Healthcare Services: Review and Future Research Directions”. Decision Sciences 19(4):889-919
Ulrich, R. S. 2001. “Effects of Healthcare Environmental Design on Medical Outcomes”. In Proceedings of the Second International Conference on Health and Design, 49-59. Stockholm, Sweden: Svensk Byggtjanst.
Ulrich, R. S., C. Zimring, X. Zhu, J. DuBose, H.-B. Seo, Y.-S. Choi, X. Quan, and A. Joseph. 2008. “A Review of the Research Literature on Evidence-based Healthcare Design”. HERD: Health Environments Research & Design Journal 1(3):61-125.
Vaughn, J. E., S. A Buckley, and R. B. Walter. 2016. “Outpatient Care of Patients with Acute Myeloid Leukemia: Benefits, Barriers, and Future Considerations”. Leukemia Research 45:53-58.
Zeigler, B. P., T. G. Kim, and H. Praehofer. 2000. Theory of Modeling and Simulation. Orlando, FL: Academic Press.
